What is obstructive sleep apnea?
Sleep apnea is a serious sleep disorder that occurs when a person's breathing is interrupted during sleep. People with untreated sleep apnea stop breathing many times during sleep, sometimes hundreds of times during the night.
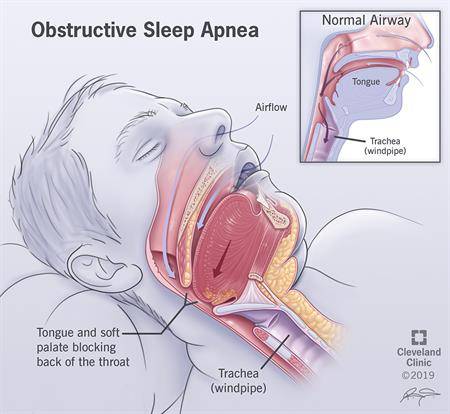
There are three types of sleep apnea: obstructive, central and mixed. Obstructive sleep apnea (OSA) is the more common of the three. Obstructive sleep apnea occurs when the upper airway is blocked either partly or completely during sleep. During an apnea episode, the diaphragm and chest muscles work harder as the pressure increases to open the airway. Breathing usually resumes with a loud gasp or body jerk. These episodes can interfere with sound sleep, reduce the flow of oxygen to vital organs, and cause heart rhythm problems.
In central sleep apnea, the airway is not blocked but the brain fails to signal the muscles to breathe due to instability in the respiratory control center. Central apnea is related to the function of the central nervous system and not treated by oral appliance therapy.
Mixed sleep apnea is a combination of both obstructive and central sleep apnea.
Who gets obstructive sleep apnea?
Obstructive sleep apnea occurs in about 25 percent of men and nearly 10 percent of women. Obstructive sleep apnea can affect people of all ages, including babies and children and particularly people over the age of forty and those who are overweight. Certain physical traits and clinical features are common in patients with obstructive sleep apnea. These include excessive weight, large neck, and structural abnormalities reducing the diameter of the upper airway, such as nasal obstruction, a low-hanging soft palate, enlarged tonsils, or a small jaw with an overbite.
What causes obstructive sleep apnea?
Obstructive sleep apnea is caused by a blockage of the airway, usually when the soft tissue in the rear of the throat collapses during sleep. Central sleep apnea is usually observed in patients with central nervous system dysfunction, such as those who have had a stroke or who have neuromuscular diseases. It is also common in patients with heart failure and other forms of cardiac and pulmonary disease.
What are the symptoms of obstructive sleep apnea?
Often the first signs of obstructive sleep apnea (OSA) are recognized not by the patient, but by the bed partner. Many of those affected have no sleep complaints. The most common symptoms of OSA include:
- Snoring
- Daytime sleepiness or fatigue
- Restlessness during sleep
- Sudden awakenings with a sensation of gasping or choking
- Dry mouth or sore throat upon awakening
- Intellectual impairment, such as trouble concentrating, forgetfulness, or irritability
- Night sweats
- Sexual dysfunction
- Headaches
Symptoms in children may not be as obvious and include:
- Poor school performance
- Sluggishness or sleepiness, often misinterpreted as laziness in the classroom
- Daytime mouth breathing and swallowing difficulty
- Inward movement of the ribcage when inhaling
- Unusual sleeping positions, such as sleeping on the hands and knees, or with the neck hyper-extended
- Excessive sweating at night
- Learning and behavioral disorders
- Bedwetting
What are the effects of obstructive sleep apnea (OSA)?
If left untreated, obstructive sleep apnea can result in a number of health problems including hypertension, stroke, arrhythmias, cardiomyopathy (enlargement of the muscle tissue of the heart), congestive heart failure, diabetes, and heart attacks. In addition, untreated sleep apnea may be responsible for job impairment, work-related accidents, and motor vehicle crashes as well as academic underachievement in children and adolescents.
What if I have been diagnosed with obstructive sleep apnea (OSA)?
If your doctor has found that you have OSA, you will be offered treatment options. Generally, the gold standard for treating OSA is a continuous positive airway pressure (CPAP) machine. For various reasons, CPAP may not work for you. Another option is oral appliance therapy which resembles a mouth guard used by athletes.
PROCEDURE DETAILS
How does oral appliance therapy work to treat obstructive sleep apnea (OSA)?
For patients with mild to moderate obstructive sleep apnea, dental appliances or oral mandibular advancement devices that prevent the tongue from blocking the throat and/or advance the lower jaw forward can be made. These devices help keep the airway open during sleep. A sleep specialist and dentist with expertise in oral appliances for this purpose should jointly determine if this treatment is best for you.
How do I order an oral appliance for obstructive sleep apnea (OSA)?
If you and your doctor decide that an oral device is a good option, you will need a referral to an appropriate dentist to have an evaluation. The dentist will decide if you are a candidate for this treatment and make an impression of your teeth. The dentist will make the device and call you back for a fitting. You will also be given a morning repositioner to realign your bite after the appliance is removed. He or she will also give you instructions on how to use and clean the appliance. You might also have to go back to the dentist for further custom adjustments to optimize care. Once care is completed, it is recommended that have another sleep test to see how the appliance is working for you. Further adjustments may be necessary.
RISKS / BENEFITS
What are the risks of oral appliance therapy for obstructive sleep apnea (OSA)?
The risks of oral appliance therapy include:
- Bite changes
- Pain in the jaw, teeth, and temporomandibular joint (TMJ) pain
- Loose teeth
- A need for dental work replacement
- Excessive drooling
- Mouth dryness
What are the benefits of oral appliance therapy for obstructive sleep apnea (OSA)?
Oral appliance therapy:
- Can improve symptoms of OSA, including daytime sleepiness, moodiness, concentration issues and reduce or eliminate snoring.
- Offers another option for people who cannot tolerate CPAP
- Is easier to take along when traveling
- Works without electricity
- Is quiet
WHEN TO CALL THE DOCTOR
What questions should I ask my doctor and dentist about an oral appliance to treat obstructive sleep apnea (OSA)?
- How much does oral appliance therapy cost?
- Will oral appliance therapy be covered by medical or dental insurance?
- What kinds of problems should I be looking for?
- How many visits will this require?
- How many sleep tests will I need to take?
- How long will the device last?
- Are there things that I should avoid doing or eating?