A consultant Obstetrician and Gynecologist and Medical Director, May Fair Specialist Hospital, Onitsha, Anambra State, Dr. Raphael Nosike Omaliko, has given reasons ovarian and uterine cancers are on the rise, especially among black women.
Ovarian, uterine (endometrial) and cervical cancers are the most common gynaecologic cancers, which begin in the female reproductive organs. Less common gynaecologic cancers involve vulva, Fallopian tube, uterine wall (sarcoma), vagina, and placenta (pregnancy tissue: molar pregnancy).
Ovarian cancer refers to any cancerous growth that begins in the ovary. This is the part of the female body that produces eggs. Feeling full too quickly or difficulty eating, bloating, and abdominal or back pain are common only for ovarian cancer.
Endometrial cancer is cancer that affects the womb. The womb (uterus) is where a baby grows during pregnancy. The most common symptom of endometrial cancer is abnormal vaginal bleeding, ranging from a watery and blood-streaked flow to a flow that contains more blood.
Pelvic pain or pressure is common for ovarian and uterine cancers.
Endometrial cancer is one of the most curable of the gynaecologic cancers because most patients have well-differentiated tumours and localised disease.
Omaliko, who is also a Fellow of International College of Surgeon, in an interview with The Guardian said uterine and ovarian cancers may eventually become the third and fourth most common type among women.
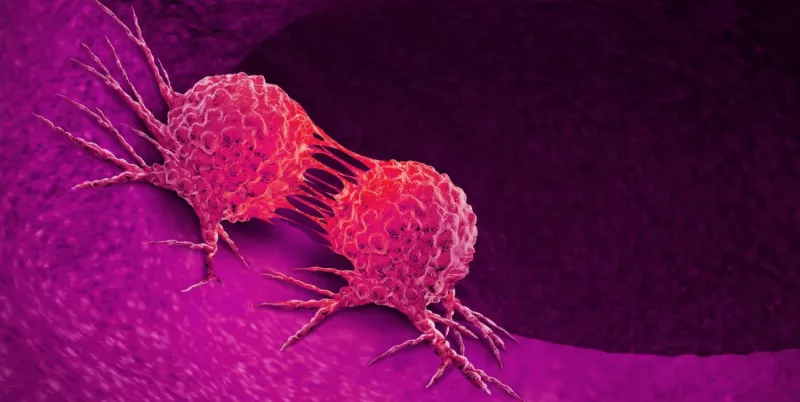
The gynaecologist explained: “Cancer is a decease in which abnormal cells divide uncontrollably, and destroy normal body tissues.

“Ovarian cancer, is a very insidious disease that occurs in women, it comes in a gradual form. Since 1930, it has had an upsurge and it’s still increasing in incidents. The incidence in the United States of America (USA) is about 0.05 percent, it presents mainly in the middle ages, between 55 and 60 years of age and it is usually detected in a very late stage. In 75 per cent of cases, it is already in the third or fourth stage which are the late stages.”
According to Omaliko, some risk factors of ovarian cancer are: reduce family size (a woman who has very few children); later age of first conception (that is women who postpone getting pregnant or married); then family history; possible links with the use of fertility drugs; radiation; and higher social economic status. He said white women are more susceptible to the cancer of the ovary and blood group A is also a risk factor in increasing the occurrence of ovarian cancer.
Omaliko, however, said some factors have been known to reduce the risk factors such as a longterm use of oral conceptive pills, which reduce ovulation and the incidence of ovarian cancer. “Multiparous women (women with many children), have been found to have less incidence of ovarian cancer, breastfeeding, women who breast feed their children, in this case are less likely to have ovarian cancer. Lower social economic status (women who are poor in the society) have less incidence as well. Japanese, Hispanic, Chinese and blacks, have also been discovered to have less incidence of ovarian cancer. Blood group O also is a factor that can reduce the incidence of ovarian cancer,” he said.
Studies have shown that cancer of the uterus, also called endometrial cancer, is increasing so rapidly that it is expected to displace colorectal cancer by 2040 as the third most common cancer among women, and the fourth-leading cause of women’s cancer deaths.
The mortality rate has been increasing by almost two percent a year overall, with even sharper spikes among Asian, Hispanic and Black women, according to a recent study in JAMA Oncology. Despite the increase, there has been little public attention to the disease.
Overall survival rates are high when uterine cancer is detected early, but few women are aware that a change in menstrual bleeding, before or after menopause, is one of the main warning signs, along with pelvic pain and painful urination and intercourse.
Uterine cancer was long believed to be less common among Black women. But newer studies have confirmed that it is not only more likely to strike Black women, but also more likely to be deadly.
Black women die of uterine cancer at twice the rate of white women, according to a report in March from an expert panel convened by the American College of Obstetricians and Gynecologists.
The gap is one of the largest racial disparities observed for any cancer, the report said. Black women are also more likely to develop a form called non-endometrioid uterine cancer, which is more aggressive.